Finding out you have cancer can be terrifying and stressful. It can be empowering to know what to anticipate, from diagnosis to recovery, and to take charge of your health. This provides a comprehensive review of cancer, including what it is, warning signs to look out for, diagnosis methods,
What is cancer?
Cancer is a large group of diseases with one thing in common: They all happen when normal cells become cancerous cells that multiply and spread.
Cancer is the second most common cause of death in the U.S. But fewer people are dying of cancer now than 20 years ago. Early detection and innovative treatments are curing cancer and helping people with cancer live longer. At the same time, medical researchers are identifying independent risk factors linked to developing cancer to help prevent people from developing cancer.
What is the difference between a normal cell and a cancerous cell?
Normally, cells follow instructions provided by genes. Genes set down rules for cells to follow, such as when to start and stop growing. Cancerous cells ignore the rules that normal cells follow:
- Normal cells divide and multiply in a controlled manner. Cancerous cells multiply uncontrollably.
- Normal cells are programmed to die (apoptosis). Cancerous cells ignore those directions.
- Normal cells for solid organs stay put. All cancerous cells are able to move around.
- Normal cells don’t grow as fast as cancerous cells.
How does cancer start in your body?
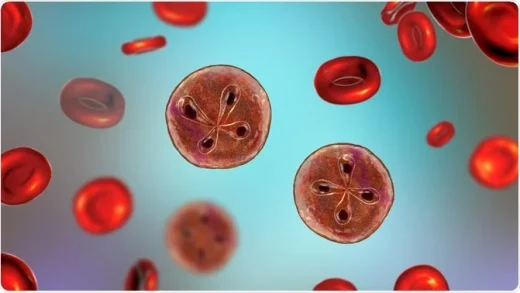
Cancer starts when a gene or several genes mutate and create cancerous cells. These cells create cancer clusters, or tumors. Cancerous cells may break away from tumors, using your lymphatic system or bloodstream to travel to other areas of your body. (Healthcare providers call this metastasis.)
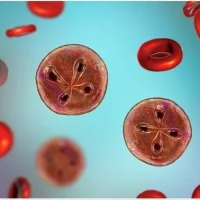
For example, a tumor in your breast may spread to your lungs, making it hard for you to breathe. In some types of blood cancer, abnormal cells in your bone marrow make abnormal blood cells that multiply uncontrollably. Eventually, the abnormal cells crowd out normal blood cells.
How common is cancer?
According to the American Cancer Society, 1 in 2 men and people assigned male at birth (AMAB) and 1 in 3 women and people assigned female at birth (AFAB) will develop cancer. As of 2019, more than 16.9 million people in the U.S. were living with cancer. The most common cancers in the United States are:
- Breast cancer: Breast cancer is the most common type of cancer. It mostly affects women and people AFAB. But about 1% of all breast cancer cases affect men and people AMAB.
- Lung cancer: Lung cancer is the second most common cancer. There are two types of lung cancer: non-small cell cancer and small cell lung cancer.
- Prostate cancer: This cancer affects 1 in 9 men and people AMAB.
- Colorectal cancer: Colon cancer and rectal cancer affect different parts of your digestive system.
- Blood cancers: Leukemia and lymphoma are the most common blood cancers.
Who’s affected by cancer?
Almost anyone may develop cancer, but data show cancer cases vary based on race and sex. According to the 2022 Annual Report on Cancer, the disease:
- Affects slightly more men and people AMAB than women and people AFAB.
- Affects more Black men (AMAB) than people in other racial groups.
- Affects more women (AFAB) who are American Indian or Alaska natives than people in other racial groups.
Almost anyone may develop cancer, but it typically affects people aged 60 and older.
Symptoms and Causes
What are cancer symptoms?
Cancer is a complicated disease. You can have cancer for years without developing symptoms. Other times, cancer may cause noticeable symptoms that get worse very quickly. Many cancer symptoms resemble other, less serious illnesses. Having certain symptoms doesn’t mean you have cancer. In general, you should talk to a healthcare provider anytime there’s a change in your body that lasts for more than two weeks.
First symptoms of cancer
Some common early cancer symptoms include:
- Unexplained weight loss.
- Chronic tiredness.
- Persistent pain.
- Fever that occurs mostly at night.
- Skin changes, particularly moles that change shape and size or new moles.
Left untreated, cancer may cause additional symptoms, including:
- Bruising or bleeding more easily.
- Lumps or bumps under your skin that don’t go away.
- Difficulty breathing.
- Difficulty swallowing.
What causes cancer?
Cancer is a genetic disorder. It happens when genes that manage cell activity mutate and create abnormal cells that divide and multiply, eventually disrupting how your body works.
Medical researchers estimate 5% to 12% of all cancers are caused by inherited genetic mutations that you can’t control.
More frequently, cancer happens as an acquired genetic mutation. Acquired genetic mutations happen over the course of your life. Medical researchers have identified several risk factors that increase your chance of developing cancer.
Cancer risk factors you can control
- Smoking: Smoking cigarettes and cigars and using e-cigarettes increases your chance of developing lung, pancreatic, esophageal and oral cancer.
- Diet: Eating high-fat or high-sugar foods can increase your risk for many types of cancer. You’re also more vulnerable to disease if you don’t get enough exercise.
- Environment: Exposure to toxins in your environment — such as asbestos, pesticides and radon — can eventually lead to cancer.
- Radiation exposure: Ultraviolet (UV) radiation from the sun significantly increases your risk of developing skin cancer. Over-exposure to radiation treatment can also be a risk factor.
- Hormone therapy: Women and people AFAB taking hormone replacement therapy may have an increased risk for breast cancer and endometrial cancer.
How can I reduce my risk of developing cancer?
You can reduce your risk by changing some of your lifestyle choices:
- If you smoke or use tobacco, try to stop. Ask a healthcare provider about smoking cessation programs that can help you quit tobacco.
- Follow a diet plan that’s healthy for you. If you want help managing your weight, ask a healthcare provider about nutritional guidance and weight management programs.
- Add exercise to your daily routine. Exercise may boost your immune system so it provides more protection against cancer.
- Avoid toxins, including asbestos, radon and pesticides.
- Protect yourself against sun damage.
- Have regular cancer screenings.
Diagnosis and Tests
How do healthcare providers diagnose cancer?
Healthcare providers begin a cancer diagnosis by doing a comprehensive physical examination. They’ll ask you to describe your symptoms. They may ask about your family medical history. They may also do the following tests:
- Blood tests.
- Imaging tests.
- Biopsies.
Blood tests
Blood tests for cancer may include:
- Complete blood count (CBC): A CBC test measures and counts your blood cells.
- Tumor markers: Tumor markers are substances that cancer cells release or that your normal cells release in response to cancer cells.
- Blood protein tests: Healthcare providers use a process called electrophoresis to measure immunoglobulins. Your immune system reacts to certain cancers by releasing immunoglobulins.
- Circulating tumor cell tests: Cancerous tumors may shed cells. Tracking tumor cells helps healthcare providers monitor cancer activity.
Imaging tests
Imaging tests may include:
- Computed tomography (CT) scan: CT scans check for cancerous tumors’ location and impact on your organs and bones.
- X-rays: X-rays use safe amounts of radiation to create images of your bones and soft tissues.
- Positron emission test (PET) scan: PET scans produce images of your organs and tissues at work. Healthcare providers may use this test to detect early signs of cancer.
- Ultrasound: An ultrasound uses high-intensity sound waves that show structures inside of your body.
- Magnetic resonance imaging (MRI): MRIs use a large magnet, radio waves and a computer to create images of your organs and other structures inside of your body.
- Iodine metaiodobenzylguanidine (MIGB): This nuclear imaging test helps detect cancer, including carcinoid tumors and neuroblastoma.
Biopsies
A biopsy is a procedure healthcare providers do to obtain cells, tissue, fluid or growths that they’ll examine under a microscope. There are several kinds of biopsies:
- Needle biopsy: This test may be called a fine needle aspiration or fine needle biopsy. Healthcare providers use a thin hollow needle and syringe to extract cells, fluid or tissue from suspicious lumps. Needle biopsies are often done to help diagnose breast cancer, thyroid cancer or cancer in your lymph nodes.
- Skin biopsy: Healthcare providers remove a small sample of your skin to diagnose skin cancer.
- Bone marrow biopsy: Healthcare providers remove a small sample of bone marrow so they can test the sample for signs of disease, including cancer in your bone marrow.
- Endoscopic or laparoscopic biopsy: These biopsies use an endoscope or laparoscope to see the inside of your body. With both of these methods, a small cut is made in your skin and an instrument is inserted. An endoscope is a thin, flexible tube with a camera on the tip, along with a cutting tool to remove your sample. A laparoscope is a slightly different scope.
- Excisional or incisional biopsy: For these open biopsies, a surgeon cuts into your body and either the entire tumor is removed (excisional biopsy) or a part of the tumor is removed (incisional biopsy) to test or treat it.
- Perioperative biopsy: This test may be called a frozen section biopsy. This biopsy is done while you’re having another procedure. Your tissue will be removed and tested right away. Results will come in soon after the procedure, so if you need treatment, it can start immediately.
Genetic testing
A single gene mutation or multiple genes that function together can cause cancer. More than 400 genes have been linked by researchers to the development of cancer. Individuals who receive these genes from their biological parents might be more susceptible to cancer. If you have an inherited type of cancer, your doctor might suggest genetic testing. In order to treat cancer, they might also use genetic testing to target particular cancer genes. They create a diagnosis based on test results. Your diagnosis will be given a number or stage by them. The greater the number, the greater the spread of cancer.
How is cancer stage determined?
Systems for staging cancer are used by medical professionals to plan treatments and create prognoses, or expected results. The most popular method for staging cancer is TNM. T represents the principal tumor. N, which stands for lymph nodes, denotes whether or not your lymph nodes have been affected by a tumor. M is for metastasis, or the spreading of cancer.
What are the four stages of cancer?
Most cancers have four stages. The specific stage is determined by a few different factors, including the tumor’s size and location:
- Stage I: The cancer is localized to a small area and hasn’t spread to lymph nodes or other tissues.
- Stage II: The cancer has grown, but it hasn’t spread.
- Stage III: The cancer has grown larger and has possibly spread to lymph nodes or other tissues.
- Stage IV: The cancer has spread to other organs or areas of your body. This stage is also referred to as metastatic or advanced cancer.
There is a Stage 0 even though stages one through four are the most typical. Cancer that is still confined to the original site is described in this initial stage. Most healthcare professionals classify cancers that are still in Stage 0 as pre-cancerous because they are typically easily treatable.
Management and Treatment
How do healthcare providers treat cancer?
Healthcare providers may use several different treatments, sometimes combining treatments based on your situation. Common cancer treatments include:
- Chemotherapy: Chemotherapy is one of the most common cancer treatments. It uses powerful drugs to destroy cancer cells. You may receive chemotherapy in pill form or intravenously (through a needle into a vein). In some cases, providers may be able to direct chemotherapy to the specific area affected.
- Radiation therapy: This treatment kills cancer cells with high dosages of radiation. Your healthcare provider may combine radiation therapy and chemotherapy.
- Surgery: Cancerous tumors that haven’t spread may be removed with surgery. Your healthcare provider may recommend therapy. This treatment combines surgery with chemotherapy or radiation to shrink a tumor before surgery or to kill cancer cells that may remain after surgery.
- Hormone therapy: Sometimes, providers prescribe hormones that block other cancer-causing hormones. For example, men and people AMAB who have prostate cancer might receive hormones to keep testosterone (which contributes to prostate cancer) lower than usual.
- Biological response modifier therapy: This treatment stimulates your immune system and helps it perform more effectively. It does this by changing your body’s natural processes.
- Immunotherapy for cancer: Immunotherapy is a cancer treatment that engages your immune system to fight the disease. The treatment may be called biological therapy.
- Targeted therapy for cancer: Cancer treatment known as “targeted therapy” focuses on the genetic alterations or mutations that cause healthy cells to develop into cancerous cells.
- Bone marrow transplantation: Also referred to as stem cell transplantation, this procedure substitutes healthy stem cells for damaged ones. During autologous transplantation, your own healthy stem cells are used. Allogeneic transplantation makes use of stem cells from a different donor.
What are cancer treatment side effects?
Healthcare professionals strive to balance the treatment to eradicate cancer while avoiding negative or long-term side effects. All cancer treatments, however, have adverse effects. Some medical procedures have side effects that persist years after the procedure is over. Palliative care reduces side effects and symptoms of cancer treatment for a large number of patients. The most typical adverse effects of cancer treatments are:
- Anemia.
- Nausea and vomiting.
- Fatigue.
- Pain.
Outlook / Prognosis
What is the prognosis/outlook for cancer?
More people are currently receiving cancer cures or are surviving the disease longer. Those with cancer who receive treatment and diagnosis early on typically have a good prognosis.
However, just like you, your cancer prognosis is distinct. Your medical professionals will base their prognosis on things like:
- Your general well-being.
- The nature of your cancer.
- The state of your cancer.
- How you might react to the medication.
Your prognosis is influenced by a number of factors, including your general health, the type and stage of your cancer, and how you respond to treatment.
The greatest source of information about your prognosis is your healthcare provider. They are aware of both you and your circumstances.
What are cancer survival rates?
Estimates of survival rates are derived from the experiences of sizable cohorts with various cancer types. Cancer survival rates differ according to cancer type, stage, and treatment, just like prognoses. The National Cancer Institute’s most recent data shows that six years after receiving a cancer diagnosis, 68% of patients with any type of cancer were still alive.
Living With
How do I live with cancer?
Taking care of oneself is crucial when dealing with cancer. Some ideas for self-care are as follows:
- Develop a healthy diet and exercise routine. For suggestions for a healthy menu, ask to speak with a nutritionist.
- One typical symptom and adverse effect of treatment is fatigue. Take note of your body’s needs and rest when necessary, not just when you feel like it.
- You might have cancer and not get well for a long time. That is great news, of course, but managing a chronic illness can be difficult. You may find that joining a support group or speaking with a mental health professional can help you deal with obstacles.
What is cancer survivorship?
You are a cancer survivor if you have the disease. The day you are diagnosed with cancer is the beginning of cancer survivorship, which lasts the rest of your life. If you have survived cancer, you will probably face a lot of difficulties or problems.
Cancer that comes back
Cancer treatments do not always completely eradicate cancerous cells. New malignant tumors may develop from those cells. Recurrent cancer refers to cancer that recurs in the same location as it did initially, spreads to organs and tissues far from the original site, or appears in lymph nodes nearby.
Second cancer
A new cancer is a recurrent cancer. Cancer in the same organ or part of the body can recur in people who have had first cancer, but the type of cancer that returns is different. They may also have cancer in different areas of their bodies. Second cancers are more common, as more people live longer with cancer.
Cancer fatigue
Cancer fatigue is a debilitating sense of exhaustion that does not improve with more sleep. Some patients experience persistent cancer fatigue even after their treatment is over.
Cancer pain
Certain cancer treatments can have painful, long-lasting side effects. According to one study, 39% of cancer patients who finished their treatment experienced ongoing pain. Pain that may not go away after treatment is peripheral neuropathy.
Chemotherapy brain fog
Chemotherapy brain fog, also known as “chemo brain,” is a condition where information retention and decision-making are impaired due to cancer or cancer treatment. About 75% of people receiving cancer treatment tell their healthcare providers that they have issues with memory, concentration and their ability to complete tasks.
When should I see my healthcare provider?
Discuss any problems you have with your cancer treatment with your healthcare provider. If you observe: Give your oncology team a call.
- A temperature of at least 101 degrees Fahrenheit (38.33 degrees Celsius).
- Severe headaches.
- Feels cold.
- Persistent cough.
- Breathing difficulty (dyspnea).
- Lesions inside your mouth or on your lips.
- Weight loss more than five pounds all at once.
- Vomiting excessively (three times per hour for three hours or longer).
- Blood in your feces (poop) or urine (pee).
- Severe bruises or bleeding.
What questions should I ask my healthcare provider?
Power comes from knowledge. Obtaining as much information as possible is important if you have received a cancer diagnosis. Here are some questions to ask your healthcare provider:
- Which kind of cancer have I got?
- Has my body been affected by the cancer in other places?
- Is there a genetic component to my cancer?
- How likely is it that I will survive?
- Which medical procedures would you suggest?
- What are my treatment’s advantages and disadvantages?
- How much time will the treatment require?
- Can I continue working while receiving cancer treatment?
- Will having cancer impact my ability to conceive?
- Will I have to stay in the hospital to receive my treatment?
- Is taking part in a clinical trial something I should do?