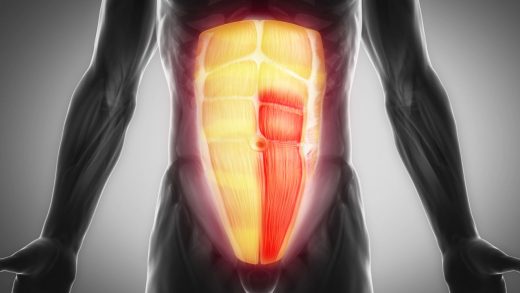
What is an abdominal aortic aneurysm?
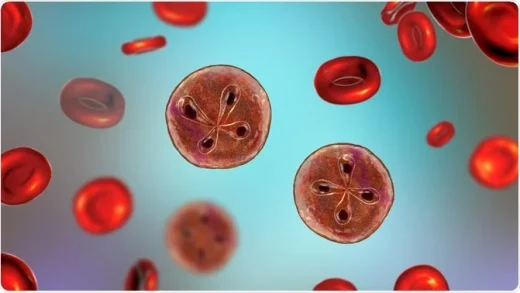
An expansion or bulge in the section of your aorta that passes through your abdomen or belly is known as an abdominal aortic aneurysm (AAA) (abdominal aorta). The weak spot in your aorta’s wall is where the bulge forms. Usually, the wall of your aorta is strong and flexible enough to handle the steady flow of blood that your heart pumps out. However, a number of things, including getting older, smoking, and having certain illnesses, can erode the wall of your aorta. The wall cannot withstand the forces of blood flow as well as it should when it is weak.
The weak spot in your aorta’s wall consequently enlarges and spreads outward. Over time, this ballooning, or expansion, keeps getting wider. If part of your aorta enlarges to 50% or more of its normal diameter, your doctor will diagnose you with a AAA. This indicates that the bulge is roughly 3 centimeters (cm) wide for most people.
Aneurysms are more likely to rupture and cause internally hemorrhaging that could be fatal the larger they get. AAAs that measure more than 5.0 centimeters in female-assigned birth cases (AFAB) and 5.5 centimeters in male-assigned birth cases (AMAB) are especially vulnerable. They get more dangerous as they get bigger. Until they rupture or are on the verge of rupturing, AAAs typically show no symptoms. To manage your risk factors for a AAA, it is crucial to find out if you have any and to collaborate with a healthcare provider.
An AAA rupture is a medical emergency. Call 911 or your local emergency number if you have sudden, severe pain in your belly or lower back. Symptoms may also include shortness of breath, dizziness, and nausea.
How common are abdominal aortic aneurysms?
Abdominal aortic aneurysms are a common condition.
- They occur in about 1.4% of adults between the ages of 50 and 84 in the U.S. This is around 1.1 million people.
- They occur in between 1% and 2% of people assigned male at birth age 65 and older. With each additional decade of life, the risk of developing an AAA doubles.
- They’re four times more common in people assigned male at birth than in people assigned female at birth.
- They occur in about 1% of people assigned female at birth who are 70 and older and have a history of smoking.
Research has also shown:
- Aneurysms can form anywhere along your aorta, but they usually form in your belly. Abdominal aortic aneurysms represent about 75% of all aortic aneurysms.
- AAAs are more common among white people compared to Black people and Asian people.
- AAAs most often affect people assigned male at birth. But when they form in people assigned female at birth, they have a higher risk of rupturing at smaller sizes as well as occurring in family members.
Symptoms and Causes
What are the symptoms of an abdominal aortic aneurysm?
Most people with an AAA don’t have symptoms until the aneurysm is close to rupturing. At that point, you may have:
- Steady, deep pain in your lower back or belly.
- Pain in your leg, groin or pelvic area.
- A pulsing sensation in your belly that feels like a heartbeat.
A ruptured AAA is a medical emergency. Symptoms begin suddenly and can include:
- Severe pain in your belly, lower back, or legs.
- Shortness of breath.
- Fast heartbeat.
- Low blood pressure.
- Dizziness or fainting.
- Nausea or vomiting.
- Clammy, sweaty skin.
Call 911 or your local emergency number if you have symptoms of an aneurysm rupture.
What causes an abdominal aortic aneurysm?
An underlying weakness in your aorta’s wall causes an AAA to form. Many environmental and hereditary factors come together to cause this weakness. Overall, the exact reason they form isn’t understood.
For instance, smoking results in the loss of structural proteins in the wall of your aorta. Its strength is diminished as a result. Another factor that can weaken the wall of your aorta is plaque accumulation, or atherosclerosis. In the layers of the artery wall, plaque development and growth over time can result in inflammation and cell death. The disintegration of the aortic wall’s building blocks makes the aorta weaker and more susceptible to abnormal expansion.
What are the risk factors for abdominal aortic aneurysms?
These risk factors play the biggest role in determining who develops an AAA:
- History of tobacco use. Researchers define this as smoking at least 100 cigarettes during your lifetime. Your exact risk varies by use (the more you use tobacco, the higher your risk).
- Older age. You face a higher risk of an AAA as you get older (over age 50 for people assigned male at birth and over age 65 for people assigned female at birth).
- Sex at birth. People assigned male at birth are more likely to develop an AAA.
- Family history of AAA. Family history plays an important role in the development of AAAs. About 10% to 20% of people who have a first-degree relative with an AAA also develop one. This means you face a higher risk if your biological parent, child or sibling had an AAA at some point in their life. The association is especially strong among brothers and siblings AMAB.
Other risk factors that can play a role include:
- High blood pressure.
- Having some form of atherosclerotic cardiovascular disease (ASCVD). This includes coronary artery disease (CAD) and peripheral artery disease (PAD).
- Having an inherited vascular connective-tissue disease.
What are the complications of AAA?
Aneurysm ruptures are the most frequent consequence, accounting for 150,000 to 200,000 deaths annually worldwide. Internal bleeding that could be fatal is caused by a ruptured AAA. When an aneurysm grows larger, your risk increases.
Diagnosis and Tests
How is an abdominal aortic aneurysm diagnosed?
Since unruptured AAAs rarely cause symptoms, medical professionals frequently identify unruptured AAAs by ordering tests for unrelated illnesses. Your provider may take the following actions if they believe you have a AAA based on test results or other factors:
- Abdominal duplex ultrasound.
- Computed tomography angiogram (CTA).
Screening for abdominal aortic aneurysms
For patients who are at risk of developing a AAA, medical professionals advise an ultrasound screening. This quick and painless imaging test determines whether you have a AAA. If so, your doctor will advise getting more ultrasounds to check on the aneurysm at regular intervals (usually every six to twelve months). Your doctor may suggest surgery if it becomes too big or if you have additional risk factors for aneurysm rupture.
Management and Treatment
What is the treatment for an abdominal aortic aneurysm?
The aneurysm’s size, which is the primary factor influencing its risk of rupturing, determines the course of treatment. Small aneurysms might not require immediate medical attention. Rather, your healthcare provider will use routine CT (computed tomography) scans or ultrasound examinations to keep an eye on the aneurysm. We refer to this strategy as surveillance. Greater aneurysms might require surgery.
Surveillance of AAAs
When the AAA measures less than 5.5 centimeters (in cases where the person was assigned male at birth) or less than 5.0 centimeters (in cases where the person was assigned female at birth), surveillance is usually warranted. Furthermore, no symptoms should be brought on by the aneurysm.
Recurrent CT or ultrasound scans will be performed on you based on the size of the aneurysm. More frequently, larger aneurysms require imaging. Instead of ultrasounds, you might receive CT scans if you are almost at the treatment threshold. Make sure you adhere to your provider’s recommendations regarding the schedule for your imaging tests. Your provider will also tell you:
- What lifestyle changes you should make. These include avoiding all tobacco use, eating a heart-healthy diet and exercising.
- Which medications you need to take to manage conditions like high blood pressure or high cholesterol.
There is currently no treatment that can shrink the aneurysm; lifestyle modifications and medication will not do this. However, taking these precautions may help lessen the growth of aneurysms and your chance of developing additional cardiovascular issues. Medication and other therapies that might restrict or halt the growth of small AAAs are still being investigated by researchers.
Surgery for AAAs
You may need surgery for your AAA if:
- The aneurysm has a diameter of at least 5.5 centimeters (in people AMAB) or 5.0 centimeters (in people AFAB). Some centers of excellence may advise elective surgery at smaller diameters depending on your overall health, risk profile and other factors.
- The aneurysm is causing symptoms, no matter its size.
- The aneurysm has ruptured. In this case, you need immediate surgery to save your life.
Surgery lowers your risk for aneurysm rupture by replacing the aorta or relining the aorta from the inside with a new graft. There are two surgical methods available to do this:
- Traditional open aneurysm repair surgery.
- Endovascular aneurysm repair (EVAR).
For elective surgery, EVAR is typically preferred by surgeons and patients due to its easier recovery and higher short-term survival rate. An EVAR can offer a durable repair when the anatomy is suitable. But you’ll need an evaluation with ultrasound or CT scans of the repair on a yearly basis. Certain factors (like your age or anatomy) may make open surgery a safer option. Each method has benefits and risks. Your provider will discuss these with you, and together, you can reach a decision.
Ruptured aneurysms need immediate surgery to give you a chance at survival.
Prevention
Can I prevent an abdominal aortic aneurysm?
There is currently no known way to stop the development of AAA. If any of your biological parents, siblings, or children had AAA, speak with your healthcare provider. To look for indications of the formation of an aneurysm, they might suggest an ultrasound screening.
You can take steps to lower other risk factors and support your overall cardiovascular health, whether or not you have a family history of AAA. Discuss with your supplier how to:
- Quit smoking or other tobacco use.
- Develop an exercise plan that’s healthy for you.
- Follow a heart-healthy diet.
- Manage your blood pressure, cholesterol, and blood sugar.
- Limit beverages containing alcohol.
Outlook and Prognosis
What can I expect if I have this condition?
Numerous variables affect your prognosis, such as the size of the aneurysm, when you receive treatment, and your general state of health. The best person to ask about future expectations is your healthcare provider. You and your particular medical history are best known to them.
Living With
How do I take care of myself?
It is crucial to take care of yourself according to your provider’s instructions if you have an AAA. They are going to customize advice for you. Here are some general pointers:
- Go to all of your medical appointments and follow-ups.
- Make lifestyle changes to support your health. Start small and give yourself reasonable goals.
- Take your medications exactly as your provider prescribes them.
- Ask your provider if you need antibiotics before certain dental or medical procedures. This is necessary for some people following aneurysm repair surgery to prevent infections.
When should I see my healthcare provider?
Call your provider if you have:
- New or changing symptoms.
- Side effects from medications.
- Questions or concerns about your condition or your treatment plan.
Your provider will tell you how often you need to come in for appointments. You may need imaging tests at regular intervals to check:
- If an AAA is growing or at risk of rupturing,.
- If there are complications from EVAR, such as an endoleak or signs of a possible re-rupture,.
Be sure to go to all of your appointments so your provider can keep an eye on your condition and help you stay healthy.
When should I go to the emergency room?
If you experience any symptoms of a AAA rupture, such as sudden, intense pain in your lower back or abdomen, call 911 or your local emergency number.
What questions should I ask my provider?
You may want to ask your provider:
- Am I at risk for an AAA?
- Do I need a screening for an AAA?
- What lifestyle changes should I make to lower my risk?
If your provider diagnosed you with an AAA, you can learn more by asking:
- How big is the aneurysm?
- Do you recommend surveillance or surgery?
- Which type of surgery is better for me?
- What are the benefits and risks of surgery?
- How long will recovery take?
- What follow-ups will I need after surgery?
- Should any of my family members have AAA screenings?
A note from DocAdvice
When you find out you have an abdominal aortic aneurysm, you may experience anxiety and worry about the future. The good news is that this aneurysm’s presence is recognized by your healthcare provider. Being aware of its existence is the first step towards maintaining your health.
When necessary, your provider will monitor your condition and make treatment recommendations. They will also advise you on ways to prevent the aneurysm from expanding or burst during your regular activities.